Top 10 Facts About Hyperplasia vs Thymoma Pathology
The thymus gland is located just below your breastbone around the upper part of your chest and is essential for normal functioning of your immune system and is very active during neonatal and childhood periods when it is producing T-lymphocytes. It is likely the birthplace of T cells, which are an absolutely important part of adaptive immunity.
however, the thymus can be subjected to diverse conditions that include thymic hyperplasia and thymoma; this can however compromise the efficiency of its function and in the end health. The pathology of these two specific conditions is a fundamental criterion that should be considered before arriving at a correct diagnosis. This article aims at depicting a caricature as well as discussing the issue of thymic hyperplasia and thymoma, highlighting the differences and similarities among them.
Thymic Hyperplasia: An Overactive Thymus
Hypertrophy of thymus: The thymus expands and becomes hyperactive, often out of proportion to the body’s needs. This may occur because of:
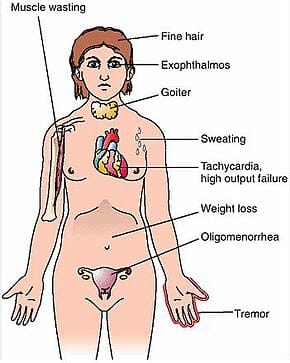
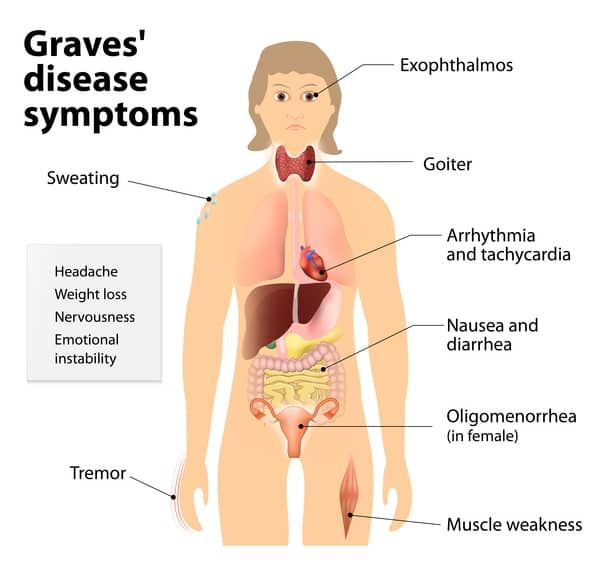
- Autoimmune diseases, like myasthenia gravis, involve the immune system attacking the body’s own tissues.
- Infections, like tuberculosis or HIV
- Certain medications, like interferon
In thymic hyperplasia, the thymus gland creates more T-cells than the body requires. This often leads to an unnecessary immune reaction. Symptoms commonly seen include:
- Fatigue
- Muscle weakness
- Difficulty swallowing
- Drooping eyelids
Thymoma: A Tumor in the Thymus
A thymoma is a rare type of tumor arising from the thymus gland. It’s usually slow-growing but can be cancerous. Thymomas develop at any age, although they are particularly more prevalent in people with advancing ages.
Thymomas can cause a range of symptoms, including:
- Chest pain or discomfort
- Coughing or difficulty breathing
- Fatigue
- Weight loss
Key Differences: Thymic Hyperplasia vs Thymoma
Here are the key differences:
- Cause: Thymic hyperplasia is usually an autoimmune disorder or an infection, while thymoma is a tumor that arises in the thymus gland.
- Growth pattern: Thymic hyperplasia causes enlargement of the thymus gland due to the hyperactivation of the immune response. In thymoma, there is a tumor in the thymus gland, and even there, it can become cancerous.
- Symptoms: While thymic hyperplasia and thymoma may cause similar symptoms, thymic hyperplasia tends to cause more systemic symptoms such as fatigue and muscle weakness while thymoma is most likely to cause localized symptoms such as chest pain and coughing.
- Treatment: Hyperplasia of the thymus as is common in patients with autoimmune disease or infection is usually treated with medications aimed to remove or control the predisposing autoimmune disorders. Thymoma can only be partially resected or in case of malignancy needs removal of the tumor via surgical means with possible radiation or chemotherapy.
Diagnosis and Treatment
Diagnosing thymic hyperplasia or thymoma, typically involves a combination of:
- Medical history and physical examination
- Imaging tests, like CT or MRI scans
- Blood tests to check for autoimmune disorders or infections
- Biopsy to examine the thymus tissue
The treatment of this pair of illnesses is commonly driven by a comprehensive strategy, which is mainly provided by immunologists, oncologists, and thoracic surgeons. Sometimes, the condition of thymectomy (a surgery to eliminate the presence of the thymus gland) is required to bring the situation under control; for example, thymic hyperplasia or thymoma.
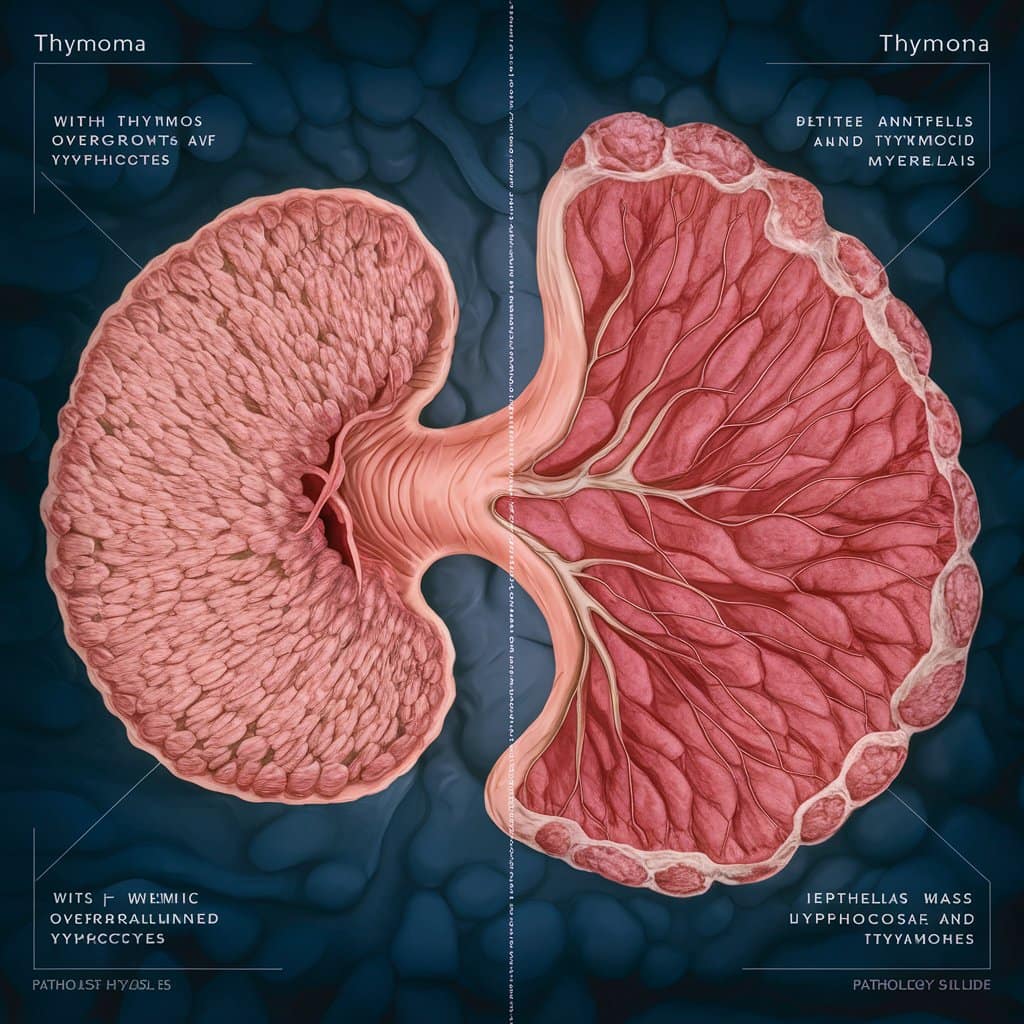
Thymic Hyperplasia Pathology Outline
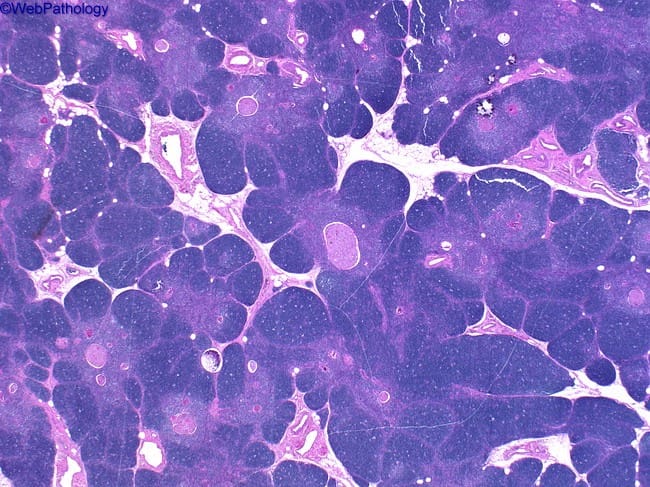
Thymic hyperplasia involves an increase in the number and size of thymic cells. It is usually a reactive process. There are two types of thymic hyperplasia: true thymic hyperplasia and lymphoid (or follicular) hyperplasia. In true thymic hyperplasia, the thymus is uniformly enlarged, and its original architecture is intact. In lymphoid hyperplasia, the thymus is filled with an abundance of lymphoid follicles with active germinal centers.
True Thymic Hyperplasia
True thymic hyperplasia frequently occurs following any factors that are related to the weakening or recovery of immunity, for instance, chemotherapy, stress, or other conditions that impact the host’s immune system. The thymic enlargement in this case can be explained as the thyroid epithelial cell and immature T-cell multiplication.
Lymphoid Hyperplasia
Thymic lymphoid hyperplasia is almost always present in the association with autoimmune diseases, such as myasthenia gravis. It is distinguishable from idiopathic thymic lymphoid hyperplasia by the presence of lymphoid follicles.
Thymoma Pathology
Thymoma is the actual neoplasm of the thymus gland—a true tumor of the thymus. Thymomas tend to be encapsulated, slow-growing, arising from the thymic epithelial cells. Unlike thymic hyperplasia, invasive thymomas tend to be encapsulated and slow-growing. Nevertheless, thymomas may invade the surrounding structures and metastasize to other parts of the body, although such occurrences are less frequent.
Features of Thymoma
Thymomas usually appear on CT scans or MRIs; a biopsy is confirmatory. Histologically, thymomas have a spectrum of appearances but contain mainly neoplastic epithelial cells and non-neoplastic lymphocytes. There are several subtypes of thymomas: thymoma “b” is further divided into morphea-like, mixed, and papillary.
Clinical Implications
Thymomas may be accompanied by syndromes of paraneoplasia, which is autoimmune phenomena that accompany tumors. About 30% of cases include myasthenia gravis, the most common condition associated with thymoma.
Thymic Hyperplasia vs. Thymoma Pathology
thymic hyperplasia and thymoma must be distinguished since treatment depends on the differentiation of the two conditions. In most cases, the condition of thymic hyperplasia is self-resolving or responded to by some treatment of the underlying condition. Thymoma may require surgical intervention.
Differences in Pathology
The process of thymic hyperplasia might involve the preservation of the usual descriptive feature of the thymus under the microscope. A growing number of cells in size is sequential and doesn’t affect the tissue’s architecture temporarily. Despite this, thymoma leads to changes in normal structure which occurs through an invasion of malignant epithelial cells.
Thymomas may also appear with areas that interrupt normal cellular structure, disrupted by necrosis and hemorrhage, also with capsules that is frequently broken down by cancer cells.
Clinical Presentation
Patients with thymic hyperplasia typically report no symptoms relating to the hyperplastic thymus. Symptoms are usually secondary to the accompanying autoimmune condition. In cases of thymoma, symptoms may be more related, such as chest pain, cough, or shortness of breath, to compression of surrounding structures.
Treatment Approaches
The mainstay of the treatment of thymic hyperplasia is the underlying cause, for example, corticosteroids for autoimmune disorders. Treatment for thymoma includes radical excision of the tumor along with complete radiotherapy or chemotherapy for aggressive, or disseminated tumors.
Diagnosis and Management
Both thymic hyperplasia and thymoma require a specific diagnosis, which is usually clinical. Treatment of these maladies depends upon the diagnosis of the condition, which involves imaging studies followed by histopathological examination, and the general health of the patient.
Diagnostic Tools
- Imaging: CT scans and MRIs are useful for identifying thymic abnormalities.
- Histopathology: After conducting the biopsy, the thymic cells are meticulously analyzed, which is the key factor that helps in distinguishing between hyperplasia and thymoma.
- Blood Tests: Immune tests can look at levels of some autoimmune indicators associated with thymic changes.
Management Strategies
- Monitoring: Observation may be the course of action for asymptomatic thymic hyperplasia.
- Medical Therapy: Treatment of underlying autoimmune conditions or the use of corticosteroids is part of managing thymic hyperplasia.
- Surgical Intervention: For thymoma, surgery to remove the tumor is the primary treatment option.
- Adjuvant Therapy: Radiation or chemotherapy may be used in the treatment of thymoma, especially if it has spread or if there are concerns about its aggressiveness.
Conclusion
in conclusion, thymic hyperplasia and thymoma owing to different properties are quite obvious. Thymic hyperplasia is a well-known type of aneurysm, especially when the immune system has already been activated. It more often than fewer causes the lack of symptoms and can disappear by itself.