Recurrence of papillary thyroid cancer post-total thyroidectomy might seem surprising, given the radical approach of removing the entire thyroid gland. Yet, it is a challenging reality that affects a significant subset of patients. This recurrence necessitates a continuous and vigilant follow-up regimen to detect and manage any returning cancer cells effectively.
Historically, the recurrence rates hover around 20-30%, which necessitates a robust understanding among healthcare professionals. Monitoring includes serum thyroglobulin levels and periodic ultrasounds, crucial tools in early detection of recurrence. The therapeutic arsenal further encompasses radioiodine treatment and in some cases, re-operative surgery, underscoring the complex landscape of managing recurrent papillary thyroid cancer.
Understanding Papillary Thyroid Cancer and Total Thyroidectomy
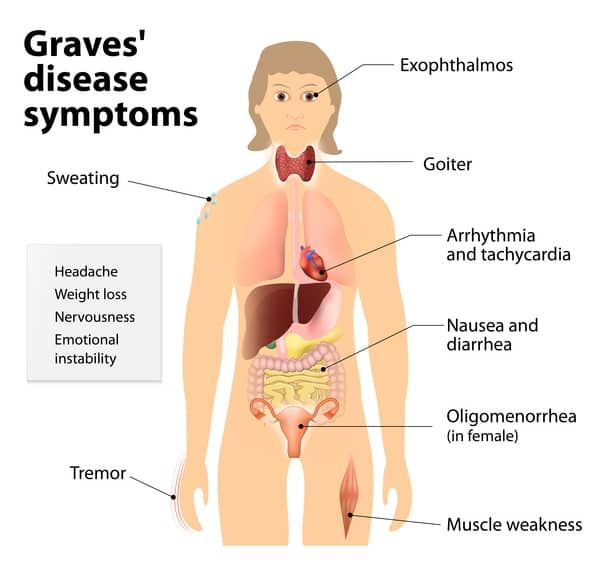
**Papillary thyroid cancer** is the most common type of thyroid cancer. It arises from the follicular cells of the thyroid gland. The disease is often curable, especially when caught early.
**Total thyroidectomy** involves the complete removal of the thyroid gland. This procedure is commonly recommended for patients with papillary thyroid cancer. Its main goal is to remove the entire cancerous tissue.
The connection between papillary thyroid cancer and total thyroidectomy is crucial for treatment. Removing the thyroid gland significantly reduces the risk of cancer spreading. This surgical approach provides a clean slate for further treatment.
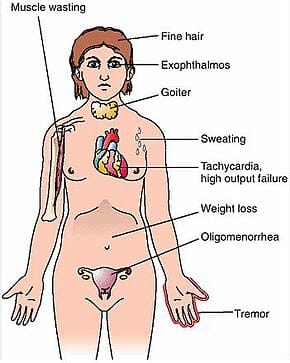
After a total thyroidectomy, patients must take lifelong thyroid hormone replacement therapy. This is because the body no longer produces thyroid hormones naturally. This therapy helps regulate the body’s metabolism.
Surviving Thyroid Cancer: 1 Year Later (Patient Testimonial Update: Erica Ervin)
Recurrence Rates of Papillary Thyroid Cancer Post-Total Thyroidectomy
After a total thyroidectomy, there still exists a chance for **papillary thyroid cancer (PTC)** to recur. This can be surprising, given the thoroughness of the surgery. However, recurrence rates typically range around 20-30%.
Several factors can influence these recurrence rates. Notably, the size and spread of the original tumor play a significant role. Advanced age and incomplete removal of cancerous tissue also increase the risk.
Diagnostic techniques like ultrasound and thyroglobulin tests are crucial in detecting recurrence. These help identify hidden cancer cells in the neck or other areas. Early detection is key to effective management.
In considering recurrence, ongoing monitoring remains essential. Regular follow-ups with the healthcare team are crucial. This approach helps manage and mitigate the risk of recurrence.
Factors Affecting Recurrence Rates
The risk of recurrence is not uniform for all patients. Specific factors significantly affect recurrence rates. The size and spread of the original tumor are critical elements.
Additionally, an older age at diagnosis increases the recurrence risk. This is because older patients might have a less robust immune response. Incomplete removal of the cancerous tissue during surgery is another significant factor.
Another consideration is the pathological features of the tumor. Tumors that invade lymph nodes or blood vessels have higher recurrence rates. Aggressive tumor characteristics warrant closer post-operative monitoring.
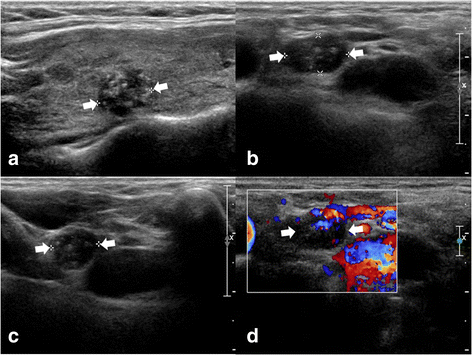
Diagnostic Techniques for Detecting Recurrence
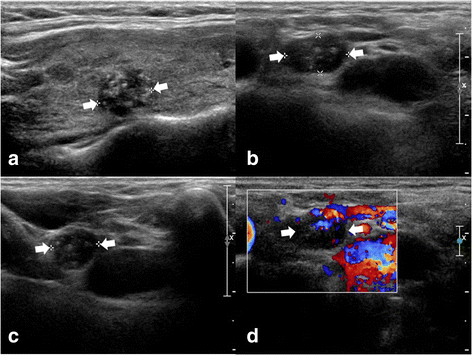
To monitor for recurrence, doctors use various diagnostic tools. Regular ultrasound scans of the neck help detect any abnormal tissue growth. Ultrasounds can reveal small, otherwise unnoticed nodules.
Serum thyroglobulin tests are another critical diagnostic tool. This protein is produced by thyroid cells, and its presence after surgery suggests recurrence. Frequent testing ensures early detection.
Radioiodine scans also play a role in detecting recurrence. Patients are given a small dose of radioactive iodine, which highlights cancer cells in imaging. This method helps detect cancer spread beyond the neck.
Strategies for Reducing Recurrence Risk
Preventing recurrence requires a multi-faceted approach. A combination of surgical precision and ongoing patient management is essential. Timely and meticulous surgeries reduce the likelihood of residual cancer cells.
Long-term use of thyroid hormone replacement therapy helps suppress cancer growth. This therapy reduces the stimulation of potential residual thyroid tissue. It acts as a preventive measure against recurrence.
Another strategy includes lifestyle changes and regular follow-up appointments. Staying attentive to health and seeking immediate medical care if symptoms arise is crucial. Regular monitoring ensures prompt intervention if cancer returns.
Diagnostic Techniques for Detecting Recurrence
Detecting the recurrence of papillary thyroid cancer (PTC) requires precise methods. Ultrasound scans are one of the primary tools used. They help by providing clear images of the neck area.
Another essential technique is the **serum thyroglobulin test**. This test measures the level of thyroglobulin in the blood, a key indicator. Persistent thyroglobulin can signal the presence of cancer cells.
**Radioiodine scans** are also significant in detecting recurrence. These scans utilize radioactive iodine to identify cancerous cells. Areas absorbing the iodine indicate possible cancer spread.
Advanced imaging methods such as **PET scans** can provide further accuracy. PET scans detect metabolic activity in tissues, pinpointing active cancer cells. These comprehensive techniques are vital for early detection.
Therapeutic Approaches in Managing Recurrent PTC
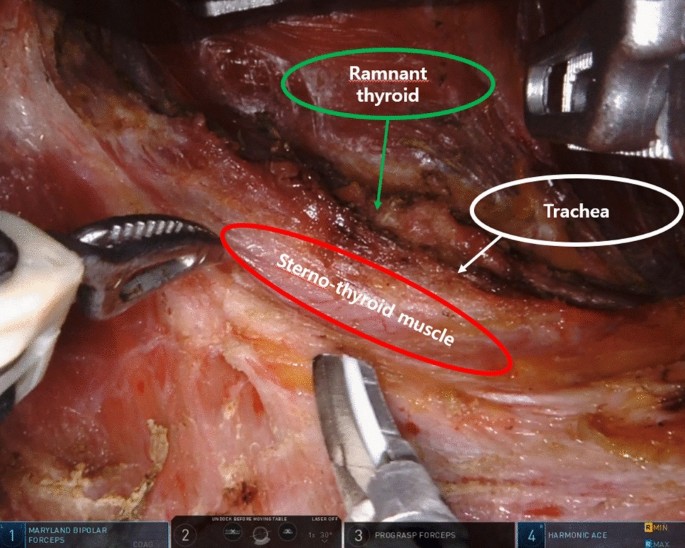
Managing recurrent papillary thyroid cancer (PTC) involves several therapeutic approaches. **Surgical intervention** is often the first step. Removing recurrent tumors can help eliminate cancerous cells.
**Radioiodine therapy** plays a crucial role in treatment. This therapy uses radioactive iodine to target and destroy cancer cells. It is particularly effective for small, localized recurrences.
**External beam radiation therapy** may be recommended for more advanced cases. This therapy uses high-energy rays to kill cancer cells. It helps reduce the size and spread of tumors.
For some patients, **systemic therapies** like chemotherapy can be beneficial. These treatments target cancer cells throughout the body. They are often used when cancer has spread beyond the thyroid area.
**Targeted therapy** is another approach that focuses on specific cancer cell mechanisms. By interfering with these mechanisms, targeted therapy aims to stop cancer cell growth. This method can be highly effective for certain genetic mutations.
Finally, **long-term monitoring** remains essential. Regular check-ups and diagnostic tests ensure early detection of any new recurrence. Proactive management helps maintain patient health.
Importance of Long-Term Follow-up
Long-term follow-up is crucial for patients with **papillary thyroid cancer (PTC)** who have undergone total thyroidectomy. Regular monitoring helps detect any signs of recurrence early. Early detection significantly improves treatment outcomes.
Typically, follow-up involves regular **physical exams** and **blood tests**. These tests measure thyroglobulin levels and other markers. Consistent testing ensures timely intervention if cancer returns.
**Ultrasound imaging** is another key component of long-term follow-up. It helps spot any abnormal growths in the neck area. This imaging technique is non-invasive and highly effective.
Patients are also encouraged to maintain an open line of communication with their healthcare team. Reporting new symptoms or concerns promptly can make a significant difference. Effective communication aids proactive management of health.
Long-term follow-up isn’t just about monitoring for cancer. It also includes ensuring effective **thyroid hormone replacement therapy**. Proper hormone levels are vital for overall well-being.
A comprehensive long-term follow-up plan enhances quality of life and health outcomes. It empowers patients to take an active role in their health care. Ongoing engagement with healthcare providers is key to successful management.
Key Takeaways
- Recurrence of papillary thyroid cancer happens in about 20-30% of cases.
- The size and spread of the initial tumor play a major role.
- Regular monitoring helps catch any recurrence early on.
- Serum thyroglobulin tests are vital for tracking potential recurrence.
- Early detection leads to better management and outcomes.
Frequently Asked Questions
Dealing with papillary thyroid cancer recurrence can be challenging. Below are some commonly asked questions and answers to help you better understand the topic.
1. What are the signs of recurrent papillary thyroid cancer?
Signs of recurrent papillary thyroid cancer often include neck swelling and difficulty swallowing. Some patients may also experience a new or persistent cough that is not associated with a cold.
If you have previously had thyroid cancer and start noticing these symptoms, it’s important to contact your healthcare provider promptly. Early detection is crucial for effective treatment.
2. How frequently should follow-up testing be done after total thyroidectomy?
The frequency of follow-up testing after a total thyroidectomy varies based on individual risk factors. Generally, it’s recommended to have serum thyroglobulin tests and neck ultrasounds every 6-12 months initially.
Your doctor will tailor the follow-up schedule to suit your specific situation. Regular monitoring helps detect any recurrence early, providing better outcomes.
3. Can lifestyle changes reduce the risk of recurrence in papillary thyroid cancer?
Lifestyle changes can play a role in managing overall health but may not directly reduce cancer recurrence risk. Maintaining a healthy diet, regular exercise, and avoiding smoking are beneficial for general well-being.
Consult your healthcare provider for personalized advice on lifestyle adjustments that could complement your medical treatments. This holistic approach can support long-term health.
4. Is radioiodine therapy effective for recurrent papillary thyroid cancer?
Radioiodine therapy is highly effective for many cases of recurrent papillary thyroid cancer, especially if detected early. The radioactive iodine targets any remaining or recurring cancer cells left behind after surgery.
The treatment is administered orally and works by selectively destroying thyroid tissue while sparing other parts of the body. Follow up sessions might be necessary depending on individual case specifics.
5. Are there alternative treatments if traditional methods do not work?
If traditional treatments like surgery and radioiodine therapy don’t work, other options exist such as targeted therapy or chemotherapy. These alternatives focus on inhibiting specific pathways that promote tumor growth.
Your medical team can guide you through the best available options tailored to your condition’s needs evolving needs and progress over time.
How common is recurrent thyroid cancer?
Conclusion
Managing papillary thyroid cancer recurrence after total thyroidectomy involves a multi-faceted approach. Regular follow-ups and diagnostic tests play a critical role in early detection. Each patient’s journey is unique, demanding personalized care and ongoing vigilance.
Therapeutic options range from surgical interventions to radioiodine therapy, and even systemic treatments. Staying proactive and engaged with healthcare providers ensures better outcomes. Continuous advancements in medical science offer hope for effective management and improved quality of life.