It’s intriguing that papillary thyroid carcinoma (PTC) is the most common type of thyroid cancer, accounting for about 80% of all cases. Despite its higher prevalence, PTC is often associated with a favorable prognosis, contributing to its reputation as a “well-behaved” malignancy. This cancer predominantly affects women and is usually detected in middle-aged adults.
The history of PTC dates back to when it was first recognized as a distinct thyroid cancer subtype due to its unique histopathological features. One remarkable aspect is the overall 10-year survival rate, which is around 90% and significantly better compared to other types of thyroid cancers. Treatment typically involves a combination of surgery, radioactive iodine therapy, and in some cases, thyroid hormone therapy, leading to excellent outcomes for most patients.
Defining Papillary Thyroid Carcinoma (PTC)
Papillary Thyroid Carcinoma (PTC) is a type of cancer that starts in the thyroid gland. The thyroid is a small gland located in the front of your neck. PTC develops from the cells that produce thyroid hormones.
This form of cancer is the most common among thyroid cancers. Interestingly, it accounts for about 80% of all thyroid cancer cases. People who get PTC are often between 30 and 50 years old.
Even though PTC affects many people, it generally has a good prognosis. Most people diagnosed with PTC live long, healthy lives. Treatment success rates are high.
Women are more likely than men to develop PTC. This cancer is usually detected early, which greatly helps in treatment. It’s essential to understand the characteristics of PTC for early diagnosis.
Understanding the Biology of PTC
Papillary Thyroid Carcinoma (PTC) starts in the thyroid gland’s follicular cells. These cells are responsible for producing and storing thyroid hormones. Changes in the DNA of these cells can lead to PTC.
Genetic mutations play a significant role in the development of PTC. Two common genes involved are BRAF and RET/PTC. These mutations can cause uncontrolled cell growth.
Environmental factors can also contribute to PTC. Exposure to radiation, especially during childhood, increases the risk. Other factors include a diet low in iodine.
The progression of PTC is usually slow. This is why the prognosis is often good with early detection and treatment. Understanding these biological aspects helps in developing better treatments.
Genetic Mutations in PTC
Genetic mutations are a driving force behind PTC. The most common mutation is in the BRAF gene. This mutation is found in about 45% of PTC cases.
The RET/PTC rearrangement is another significant mutation. This genetic change is often seen in patients exposed to radiation. It leads to the activation of pathways that promote cancer cell growth.
A third genetic factor is the TERT promoter mutation. Although less common, it is linked to more aggressive forms of PTC. Identifying these mutations can guide personalized treatment plans.
Environmental Factors
Radiation exposure is a well-known risk factor for PTC. Events like childhood radiation therapy increase the chance of developing this cancer. Nuclear accidents are another source of radiation.
A diet low in iodine can also contribute to PTC. Iodine is essential for thyroid function. Without enough iodine, the thyroid may become more susceptible to cancer.
Other environmental factors include exposure to certain chemicals. Some studies suggest a link between PTC and chemicals found in pesticides. Identifying these factors helps in prevention efforts.
Cellular Mechanisms
The cellular mechanisms of PTC involve changes in cell signaling pathways. Mutations in genes like BRAF and RET/PTC activate these pathways. This leads to uncontrolled cell division and tumor growth.
Apoptosis, or programmed cell death, is often disrupted in PTC. Cancer cells evade this process, allowing them to survive longer. This contributes to the development and progression of the cancer.
Angiogenesis, the formation of new blood vessels, also plays a role. Tumors need a blood supply to grow and spread. Understanding these mechanisms is crucial for developing targeted therapies.
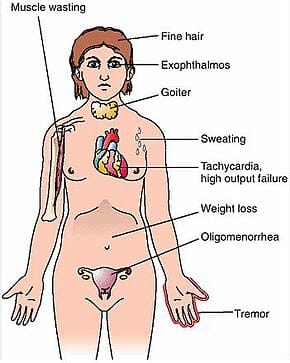
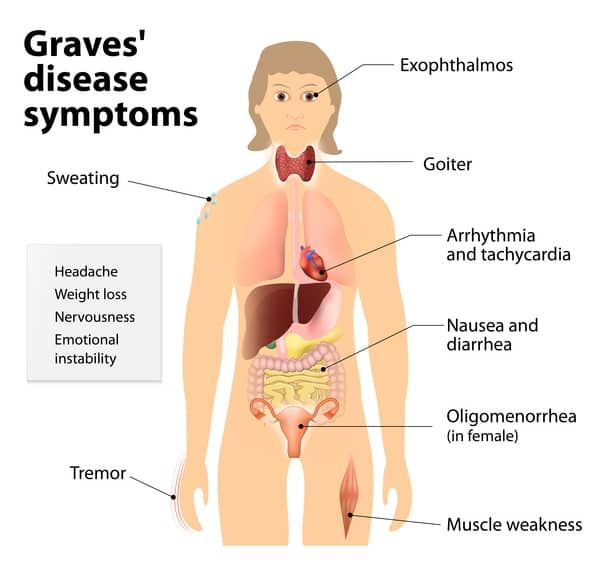
Signs and Symptoms of PTC
Papillary Thyroid Carcinoma (PTC) often presents with a noticeable lump in the neck. This lump is usually painless and can be felt just below the Adam’s apple. It’s crucial to get it checked if you notice such a lump.
Other symptoms can include hoarseness or changes in your voice. This happens when the tumor affects the vocal cords. Difficulty swallowing or a sensation that something is stuck in your throat can also occur.
People with PTC may experience swollen lymph nodes in the neck. These nodes can be a sign that the cancer has spread. When detected early, treatment becomes more effective.
Less common symptoms include persistent cough not related to a cold or allergies. Fatigue and unexplained weight loss may also be signs. Paying attention to these changes can lead to earlier diagnosis and treatment.
- Noticing a lump in the neck
- Hoarseness or voice changes
- Difficulty swallowing
- Swollen lymph nodes
- Persistent cough
Diagnostic Tests for PTC
When diagnosing Papillary Thyroid Carcinoma (PTC), an ultrasound of the neck is usually the first step. This test helps visualize the thyroid gland and detect any abnormalities. The ultrasound can locate nodules or lumps that may indicate cancer.
If a suspicious nodule is found, a fine needle aspiration biopsy (FNAB) is often performed. During this test, a thin needle is inserted into the nodule to collect cells. These cells are then examined under a microscope to check for cancerous changes.
Blood tests can also provide valuable information. These tests measure the levels of thyroid hormones and thyroid-stimulating hormone (TSH) in the blood. Abnormal levels may suggest thyroid problems, including cancer.
In some cases, doctors may recommend a radioactive iodine scan. This test involves swallowing a small amount of radioactive iodine, which the thyroid gland absorbs. Images are then taken to observe how the thyroid is functioning and detect any cancerous activity.
Advanced imaging tests like CT scans or MRIs might be used if the cancer has potentially spread. These scans provide detailed images of the body’s internal structures. They help determine the extent of the spread and guide treatment plans.
Genetic testing is another tool for diagnosing PTC. This test screens for specific genetic mutations linked to thyroid cancer. Identifying these mutations can confirm the diagnosis and help tailor treatment options.
- Ultrasound
- Fine needle aspiration biopsy (FNAB)
- Blood tests
- Radioactive iodine scan
- CT scans or MRIs
- Genetic testing
Treatment Options and Prognosis for PTC
The treatment for Papillary Thyroid Carcinoma (PTC) often begins with surgery. The most common surgical procedure is a thyroidectomy, where part or all of the thyroid gland is removed. Surgery is highly effective in eliminating the tumor.
Radioactive iodine therapy is frequently used after surgery. This treatment involves swallowing a pill containing radioactive iodine. The iodine targets and destroys any remaining cancerous thyroid cells.
Some patients may need thyroid hormone therapy after surgery. This therapy helps replace the hormones that the thyroid would normally produce. It also helps to suppress TSH, which can stimulate cancer growth.
For more advanced cases, external beam radiation therapy might be considered. This treatment uses high-energy rays to target and destroy cancer cells. It is usually reserved for cases where the cancer has spread beyond the thyroid.
- Thyroidectomy
- Radioactive iodine therapy
- Thyroid hormone therapy
- External beam radiation therapy
- Targeted drug therapy
The prognosis for PTC is generally excellent. The 10-year survival rate is about 90%, especially when detected early. Most patients live long, healthy lives after treatment.
Factors that influence prognosis include the size of the tumor and whether it has spread. Age and overall health also play a role. Regular follow-up care is essential to monitor for potential recurrence.
Key Takeaways
- Papillary thyroid carcinoma (PTC) is the most common type of thyroid cancer.
- PTC usually affects middle-aged adults more commonly than younger or older people.
- Women are more likely to develop PTC compared to men.
- The prognosis for PTC is generally good with high survival rates.
- Treatments include surgery and radioactive iodine therapy for effective management.
Frequently Asked Questions
Papillary Thyroid Carcinoma (PTC) often raises many questions. Here are some common ones to help you understand this condition better.
1. How is PTC usually detected?
PTC is often detected through a neck ultrasound. This imaging test can show any abnormalities in the thyroid gland, like nodules or lumps. If something suspicious is found, doctors may do a biopsy to confirm if it’s cancerous.
In addition to an ultrasound, blood tests measuring thyroid hormone levels can be crucial for diagnosis. The combination of these tests helps ensure that PTC is detected early for more effective treatment.
2. What are the primary risk factors for developing PTC?
The primary risk factors for PTC include exposure to radiation and having a family history of thyroid cancer. Radiation can come from medical treatments or environmental sources like nuclear accidents.
Other less common risk factors include low iodine diets and certain genetic conditions. Understanding these risks can help in taking preventive measures and seeking timely medical advice.
3. Can PTC spread to other parts of the body?
Yes, PTC can spread to other parts of the body if not diagnosed early. It most commonly spreads to nearby lymph nodes but can also reach distant organs like the lungs or bones.
However, even when it spreads, the prognosis remains good with appropriate treatment. Early detection significantly reduces the chances of the cancer spreading further.
4. Are there lifestyle changes that can reduce the risk of PTC?
A diet rich in iodine is one way to reduce the risk of developing PTC since iodine is crucial for thyroid function. Avoiding unnecessary exposure to radiation also plays a significant role in lowering risk.
Regular medical check-ups, especially if you have a family history of thyroid issues, are advisable. Simple lifestyle adjustments can make a big difference in your long-term health.
5. Is it possible to live a normal life after being treated for PTC?
Yes, it’s entirely possible to live a normal life after being treated for PTC! Most patients have excellent long-term survival rates thanks to effective treatments like surgery and radioactive iodine therapy.
You will need regular follow-up appointments with your doctor to monitor your condition. With proper care and monitoring, you can return to everyday activities without significant limitations.
Conclusion
Understanding Papillary Thyroid Carcinoma (PTC) is crucial for early detection and effective treatment. With advancements in medical technology, the outlook for PTC patients is largely positive. Timely intervention and continuous monitoring can significantly improve outcomes.
Recognizing the signs and symptoms plays a key role in prompt diagnosis. While the risk factors vary, lifestyle changes and regular check-ups can make a big difference. Knowledge and vigilance are essential in managing and overcoming PTC.