A Step-by-Step Guide to Treatment for Amiodarone-Induced Thyrotoxicosis Type 1 and Type 2
Thyrotoxicosis is a side effect of amiodarone, a drug commonly used to treat irregular heart rhythms. This side effect is quite rare but serious. Thyrotoxicosis is the condition of excessive production by the thyroid gland, which can cause a host of symptoms, including weight loss, anxiety, and a rapid heart rate. There are two types of amiodarone-induced thyrotoxicosis: Type 1 and Type 2. In this article, we will delve into the differences between these two types, their causes, symptoms, and treatment options.
What is amiodarone-induced thyrotoxicosis?
Amiodarone is a medication that contains high amounts of iodine, an essential element for the production of thyroid hormones. When taken in large doses or for extended periods, amiodarone can cause the thyroid gland to produce excessive amounts of thyroid hormones, leading to thyrotoxicosis. This condition can occur in up to 10% of patients taking amiodarone, particularly in those with a pre-existing thyroid condition.
Type 1 Amiodarone-Induced Thyrotoxicosis
Type 1 amiodarone-induced thyrotoxicosis is the most common form of the condition, accounting for approximately 70% of cases. It is caused by the excess iodine in amiodarone, which leads to an increase in thyroid hormone production. This type of thyrotoxicosis is often associated with a pre-existing thyroid condition, such as nodular goiter or thyroid autonomy.
Symptoms of Type 1 Amiodarone-Induced Thyrotoxicosis
The symptoms of Type 1 amiodarone-induced thyrotoxicosis are similar to those of hyperthyroidism, including:
- Weight loss
- Anxiety
- Insomnia
- Fatigue
- Heat intolerance
- Palpitations
- Tremors
Treatment of Type 1 Amiodarone-Induced Thyrotoxicosis
Type 1 AIT is caused by the excess iodine content in amiodarone, which leads to increased synthesis and release of thyroid hormones. This type of AIT usually occurs in patients with pre-existing thyroid disorders, such as nodular goiter or latent Graves’ disease. The excess iodine from amiodarone provides additional substrate for thyroid hormone production, leading to hyperthyroidism.
This can be achieved through:
- Beta-blockers to control symptoms
- Thionamides to reduce thyroid hormone production
- Radioactive iodine therapy to destroy excess thyroid tissue
Type 2 Amiodarone-Induced Thyrotoxicosis
Type 2 amiodarone-induced thyrotoxicosis is a less common form of the condition, accounting for approximately 30% of cases. It is caused by the destruction of thyroid cells, leading to the release of pre-formed thyroid hormones into the bloodstream. This type of thyrotoxicosis is often associated with normal or even low thyroid hormone production prior to the development of thyrotoxicosis.
Symptoms of Type 2 Amiodarone-Induced Thyrotoxicosis
Symptoms of Type 1 AIT include weight loss, heat intolerance, tremors, palpitations, and nervousness. Treatment typically involves discontinuing amiodarone and administering antithyroid drugs, such as methimazole or propylthiouracil, to reduce thyroid hormone production. In some cases, radioactive iodine therapy or
The symptoms of Type 2 amiodarone-induced thyrotoxicosis are similar to those of Type 1, including:
- Weight loss
- Anxiety
- Insomnia
- Fatigue
- Heat intolerance
- Palpitations
- Tremors
Treatment of Type 2 Amiodarone-Induced Thyrotoxicosis
Type 2 AIT is a destructive thyroiditis caused by the direct toxic effect of amiodarone on thyroid cells. This type of AIT occurs in patients with no prior thyroid disorders and is more common than Type 1 AIT. The damage to thyroid cells leads to the release of preformed thyroid hormones into the bloodstream, causing hyperthyroidism.
Treatment for Type 2 amiodarone-induced thyrotoxicosis typically involves reducing the levels of thyroid hormones in the body through:
- Glucocorticoids to reduce inflammation
- Beta-blockers to control symptoms
- Potassium perchlorate to reduce thyroid hormone production
Key Differences between Type 1 and Type 2 Amiodarone-Induced Thyrotoxicosis
Differentiating between Type 1 and Type 2 AIT can be challenging, as the symptoms are similar. However, certain tests can help in the diagnosis:
The key differences between Type 1 and Type 2 amiodarone-induced thyrotoxicosis are:
- Cause: Type 1 is caused by excess iodine, while Type 2 is caused by thyroid cell destruction
- Thyroid hormone production: Type 1 is associated with increased thyroid hormone production, while Type 2 is associated with normal or low thyroid hormone production
- Treatment: Type 1 treatment involves reducing thyroid hormone production, while Type 2 treatment involves reducing inflammation and thyroid hormone levels
- Doppler flow: In Type 1 AIT, thyroid blood flow is increased, while in Type 2 AIT, blood flow is reduced.
What are the treatment options for Type 1 amiodarone-induced thyrotoxicosis?
The treatment options for Type 1 amiodarone-induced thyrotoxicosis typically involve reducing the levels of thyroid hormones in the body and managing symptoms. The following are some of the treatment options:
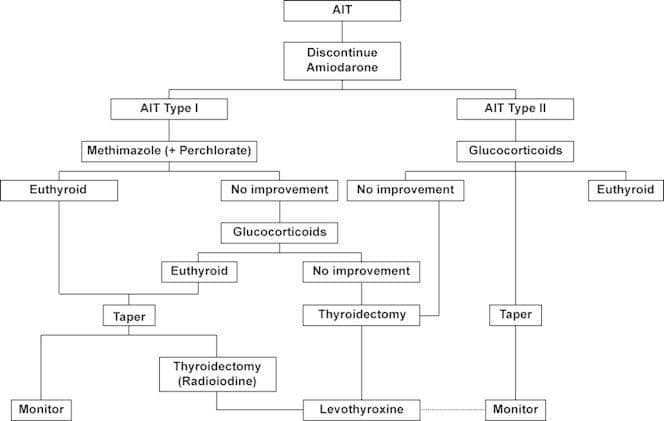
1. Discontinuation of Amiodarone:
The first step in treating Type 1 amiodarone-induced thyrotoxicosis is to stop taking amiodarone. This can help reduce the amount of iodine in the body and decrease thyroid hormone production.
2. Thionamides:
Thionamides, such as methimazole or propylthiouracil, are medications that can help reduce thyroid hormone production. They work by inhibiting the production of thyroid hormones in the thyroid gland.
3. Beta Blockers:
Beta-blockers, such as propranolol, are medications that can help manage symptoms of thyrotoxicosis, such as tremors, anxiety, and palpitations. They work by blocking the effects of excessive thyroid hormones on the body.
4. Radioactive Iodine Therapy:
Radioactive iodine therapy involves taking a small dose of radioactive iodine, which is absorbed by the thyroid gland. The radioactive iodine then destroys a portion of the thyroid gland, reducing its ability to produce thyroid hormones.
5. Thyroidectomy:
Surgical removal of the thyroid gland, or thyroidectomy, may sometimes be required in cases of Type 1 amiodarone-induced thyrotoxicosis. In general, this is saved for those patients who are refractory to other therapies or who have a large goiter.
6. Potassium Perchlorate:
Potassium perchlorate is a medication that can help reduce the amount of iodine in the body. It works by inhibiting the uptake of iodine by the thyroid gland.
7. Plasmapheresis:
Plasmapheresis is a procedure that involves removing excess thyroid hormones from the bloodstream. This can help to quickly reduce the symptoms of thyrotoxicosis.
8. Corticosteroids:
Corticosteroids, such as prednisone, may be used to reduce inflammation in the thyroid gland and surrounding tissues.
type 1 vs type 2 amiodarone-induced hyperthyroidism
Amiodarone, an antiarrhythmic drug, can cause two types of drug-induced hyperthyroidism: type 1 and type 2. Here are the main differences between the two:
Type 1 Amiodarone-Induced Hyperthyroidism (AIH):
- Mechanism: Occurs due to the excess iodine content in amiodarone, which leads to increased thyroid hormone synthesis in patients with underlying thyroid autonomy (e.g., multinodular goiter or latent Graves’ disease).
- Pathophysiology: Unregulated thyroid hormone production due to the Jod-Basedow effect (iodine-induced hyperthyroidism).
- Thyroid gland: usually preexisting thyroid abnormalities, such as nodular goiter or latent Graves’ disease.
- Iodine uptake is elevated.
- Treatment: Antithyroid drugs (e.g., methimazole or propylthiouracil) are the primary treatment. In some cases, a thyroidectomy may be necessary.
Type 2 Amiodarone-Induced Hyperthyroidism (AIH):
- Mechanism: Results from a direct toxic effect of amiodarone on thyroid follicles, with resulting destructive thyroiditis and the release of preformed thyroid hormones into the circulation.
- Pathophysiology: Thyroid follicle damage and inflammation due to amiodarone toxicity.
- Thyroid gland: There are usually no preexisting thyroid abnormalities.
- Iodine uptake is low or absent.
- Treatment: The mainstays of treatment are glucocorticoids (such as prednisone) to decrease inflammation and reduce the amount of thyroid hormone released. Iopanoic acid or potassium perchlorate may be given in certain situations to reduce the release and synthesis of thyroid hormone.
Conclusion
Amiodarone-induced thyrotoxicosis is a very rare but serious side effect of the administration of amiodarone. Making a proper differential diagnosis between Type 1 and Type 2 amiodarone-induced thyrotoxicosis is crucial to successful treatment. By identifying the symptoms and causes of each type, a doctor can easily focus treatment and improve the results for patients suffering from such a pathology.