Surprisingly, nearly 80% of all thyroid cancer cases are classified as papillary thyroid cancer, making it the most prevalent thyroid malignancy. In its initial stages, it often goes unnoticed due to the subtlety of its symptoms. This can lead to delayed diagnosis and treatment, impacting patient outcomes.
One of the most significant symptoms is a palpable, firm nodule in the neck, which can sometimes be felt during self-examination. Another critical indicator is unexplained hoarseness or a persistent cough that won’t go away. The typical age of onset is between 30 and 50 years, with women being two to three times more likely to be affected than men.
Overview of Papillary Thyroid Cancer
Papillary thyroid cancer is the most common type of thyroid cancer, making up about 80% of all thyroid cancer cases. It develops from the follicular cells in the thyroid gland. This cancer type usually grows slowly and is highly treatable.
Typically, papillary thyroid cancer affects people between the ages of 30 and 50. Women are two to three times more likely to get this type of cancer than men. This gender disparity remains a significant observation in thyroid cancer studies.
Prevalence and Risk Factors
It’s crucial to note that the exact cause of papillary thyroid cancer is still unknown. However, certain factors increase the risk, such as radiation exposure. A family history of thyroid cancer can also elevate one’s risk.
People exposed to radiation, especially during childhood, are more likely to develop it. Genetics can also play a role, making family history a significant risk factor. Lifestyle and environmental influences are still being studied for their impact.
Age and Gender Disparity
The most affected age group for papillary thyroid cancer falls between 30 and 50 years old. Women are more susceptible to this type of cancer. In fact, it’s two to three times more common in women than in men.
This gender disparity remains a focus in medical research. Understanding why women are more prone could lead to better prevention and treatment strategies. Early diagnosis is crucial for effective treatment.
Overall, papillary thyroid cancer has a high survival rate, especially when diagnosed early. Modern treatments have made significant strides in improving patient outcomes. Regular check-ups and awareness are key to early detection and management.
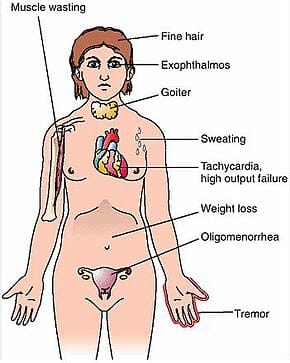
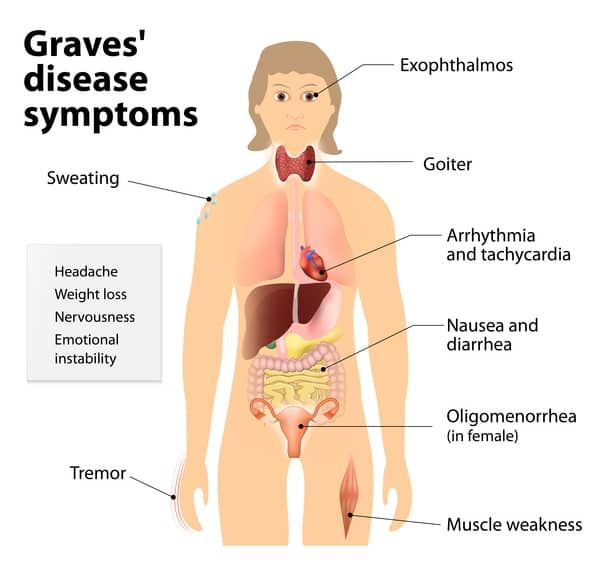
Primary Symptoms of Papillary Thyroid Cancer
Papillary thyroid cancer often shows subtle yet noticeable symptoms. Being aware of these can lead to early detection and effective treatment. Below are the primary symptoms to watch for.
Neck Nodules or Lumps
One of the earliest signs is a firm nodule or lump in the neck, usually painless. These nodules can sometimes grow large enough to be visible. It’s essential to get any suspicious lumps checked by a doctor.
A nodule that increases in size over time can be a cause for concern. It may not always mean cancer, but prompt medical evaluation is crucial. Even if pain is absent, persistent nodules warrant attention.
Unexplained Hoarseness
Another significant symptom is unexplained hoarseness or changes in the voice. If your voice becomes raspy without a clear reason, it could be a sign. This occurs because the cancer may affect the vocal cords.
Persistent hoarseness lasting more than a few weeks should be evaluated. It is especially important if hoarseness is accompanied by other symptoms. Being proactive with voice changes can lead to early intervention.
Persistent Cough and Difficulty Swallowing
A persistent cough not related to a cold or allergies is another symptom. This isn’t just an occasional cough; it’s continuous and unexplained. It happens when the cancer affects surrounding tissues.
Difficulty swallowing, also known as dysphagia, can occur. This usually means the cancer is pressing on the esophagus. Prompt medical consultation is necessary for both symptoms.
Early detection significantly improves treatment outcomes. Watching for and recognizing these symptoms can make a big difference. Always consult a healthcare provider for accurate diagnosis and care.
The Silent Nature of Papillary Thyroid Cancer
Papillary thyroid cancer is often called a “silent” disease. This is because its symptoms can be very subtle and easily overlooked. Many people don’t realize they have it until it’s advanced.
The symptoms are often painless, making it hard to detect early. A small lump or nodule in the neck might not seem alarming. Because it grows slowly, people may not notice the changes right away.
Even once symptoms appear, they may seem harmless. A mild sore throat or slight hoarseness might not raise immediate concerns. This delay in noticing signs can lead to a delayed diagnosis.
The silent nature of this cancer highlights the importance of regular medical check-ups. Being aware of subtle changes in your body can be lifesaving. Early detection is key to effective treatment and better outcomes.
Self-Examination and Detection
Regular self-examination is crucial for the early detection of papillary thyroid cancer. It helps identify symptoms that might otherwise go unnoticed. Knowing what to look for can make a significant difference.
Start by standing in front of a mirror and looking at your neck. Swallow a glass of water and observe any lumps or protrusions. Feel around your neck for any nodules or unusual changes.
If you find a lump, it’s essential not to panic. While many lumps are benign, you should consult a doctor for an accurate diagnosis. Early professional evaluation can rule out or confirm cancer.
Besides lumps, pay attention to voice changes or constant hoarseness. Persistent coughs, especially without a cold, should also be monitored. These symptoms, though subtle, can be early warning signs of thyroid issues.
Additionally, keep track of any difficulty swallowing. Even slight discomfort can be significant. Awareness of these symptoms can lead to prompt and effective treatment.
Always prioritize regular check-ups and seek medical advice if you notice anything unusual. Early detection greatly improves treatment success rates. Being proactive can save your life.
Treatment Options and their Effectiveness
Treating papillary thyroid cancer often starts with surgery. Thyroidectomy, or removal of part or all of the thyroid gland, is a common procedure. This surgery is highly effective, especially when the cancer is detected early.
In some cases, radioactive iodine therapy follows surgery. This treatment uses radioactive iodine to target and destroy remaining cancer cells. It’s effective because only thyroid cells absorb iodine, minimizing damage to other tissues.
External beam radiation therapy is another option. This treatment involves directing high-energy beams at the cancer. It’s used less commonly but can be effective for advanced cases.
Chemotherapy is less frequently used but can be an option for aggressive or recurrent cases. It involves using drugs to kill cancer cells or stop their growth. The effectiveness can vary based on individual cases.
- Thyroidectomy: High success rate when detected early.
- Radioactive Iodine Therapy: Targets thyroid cells specifically.
- External Beam Radiation Therapy: Effective for advanced stages.
- Chemotherapy: Options for aggressive or recurring cancer.
The prognosis for papillary thyroid cancer is generally favorable. Most patients respond well to treatment and can lead healthy lives. Regular follow-ups are crucial for monitoring and ensuring the cancer does not return.
Key Takeaways
- Papillary thyroid cancer often shows symptoms like a painless neck lump.
- Unexplained hoarseness or voice changes are common signs to watch for.
- Persistent cough not related to a cold can indicate thyroid issues.
- Difficulty swallowing may also be a symptom of this type of cancer.
- Early detection through regular check-ups is crucial for effective treatment.
Frequently Asked Questions
Understanding papillary thyroid cancer can be challenging, especially when it comes to its symptoms and treatments. Here are some common questions answered in a simple manner.
1. What causes papillary thyroid cancer?
The exact cause of papillary thyroid cancer is unknown. However, several risk factors can increase the likelihood of developing it. These include genetic mutations and a family history of thyroid cancer.
Exposure to high levels of radiation, especially during childhood, is another significant risk factor. Some studies also suggest that certain lifestyle and environmental factors might play a role.
2. How is papillary thyroid cancer diagnosed?
Papillary thyroid cancer is usually diagnosed through a combination of physical exams and medical imaging tests. Ultrasound is often the first tool used to examine the thyroid gland for abnormalities.
If a suspicious nodule is found, a fine needle aspiration biopsy may be performed. This involves extracting cells from the nodule for lab analysis to determine if they are cancerous.
3. Is surgery always required for treating papillary thyroid cancer?
Surgery is one of the most common treatments for papillary thyroid cancer, specifically a procedure called thyroidectomy. In some cases, only part of the gland is removed, while in others, the entire gland may need to be taken out.
After surgery, additional treatments like radioactive iodine therapy might be recommended to eliminate any remaining cancer cells. The necessity of surgery largely depends on the size and stage of the tumor.
4. Can lifestyle changes help manage papillary thyroid cancer?
Lifestyle changes can complement medical treatment but are not standalone solutions for managing papillary thyroid cancer. Maintaining a healthy diet and regular exercise can support overall well-being during treatment.
Avoiding exposure to unnecessary radiation and regular medical check-ups are crucial preventative measures. These steps may reduce risks but do not replace professional medical treatments.
5. How successful are treatments for papillary thyroid cancer?
The prognosis for papillary thyroid cancer is generally very favorable, especially if detected early. Surgical removal combined with radioactive iodine therapy has high success rates in eliminating tumors.
The survival rate for patients with early-stage diagnosis is over 90%. Regular follow-ups ensure any recurrence or complications are promptly addressed, further improving long-term outcomes.
Conclusion
Papillary thyroid cancer, though often silent and subtle in its early stages, can be effectively managed with timely detection and appropriate treatment. Regular self-examinations and being mindful of symptoms like neck nodules and voice changes are crucial. Early intervention can significantly improve outcomes and overall prognosis.
Understanding the treatment options and their effectiveness helps in making informed decisions. Whether it’s surgery, radioactive iodine therapy, or lifestyle changes, each element plays a vital role in the patient’s journey. Staying proactive in monitoring and seeking medical advice ensures the best possible care and recovery.