The Complex Relationship Between Multiple Sclerosis and Hashimoto’s Encephalopathy: Unraveling the Mysteries

Multiple sclerosis and Hashimoto’s encephalitis are pathologically very distinct autoimmune diseases that affect the CNS. While they do have certain similarities, they differ in pathophysiological mechanisms and clinical presentation. However, recently, a very interesting relationship has been established between these two conditions, showing that they are more connected than one might have thought. This paper discusses the intricacies of multiple sclerosis and Hashimoto’s encephalitis concerning their similarities and differences, together with the interesting relationship between them.
Multiple Sclerosis: An Overview
Multiple sclerosis is a chronic, disabling autoimmune disease that causes demyelination in the CNS, which affects the protective covering of the nerve fibers (myelin), resulting in disruption of the communication between the brain and the rest of the body.
Due to the mistaken attack of the myelin sheath, there is inflammation, scarring, and damage to the nerve fibers. This process results in a variety of symptoms, including loss of vision, muscle weakness, numbness or tingling, fatigue, and cognitive difficulties.
MS is heterogeneous and has different subtypes of disease and different levels of seriousness. RRMS, SPMS, and PPMS are the more usual forms of MS. Although the exact causes of MS are still not identified, the research is targeting genetic, environmental, and immune system contributions towards its development.
Hashimoto’s Encephalopathy: A Rare but Devastating Condition
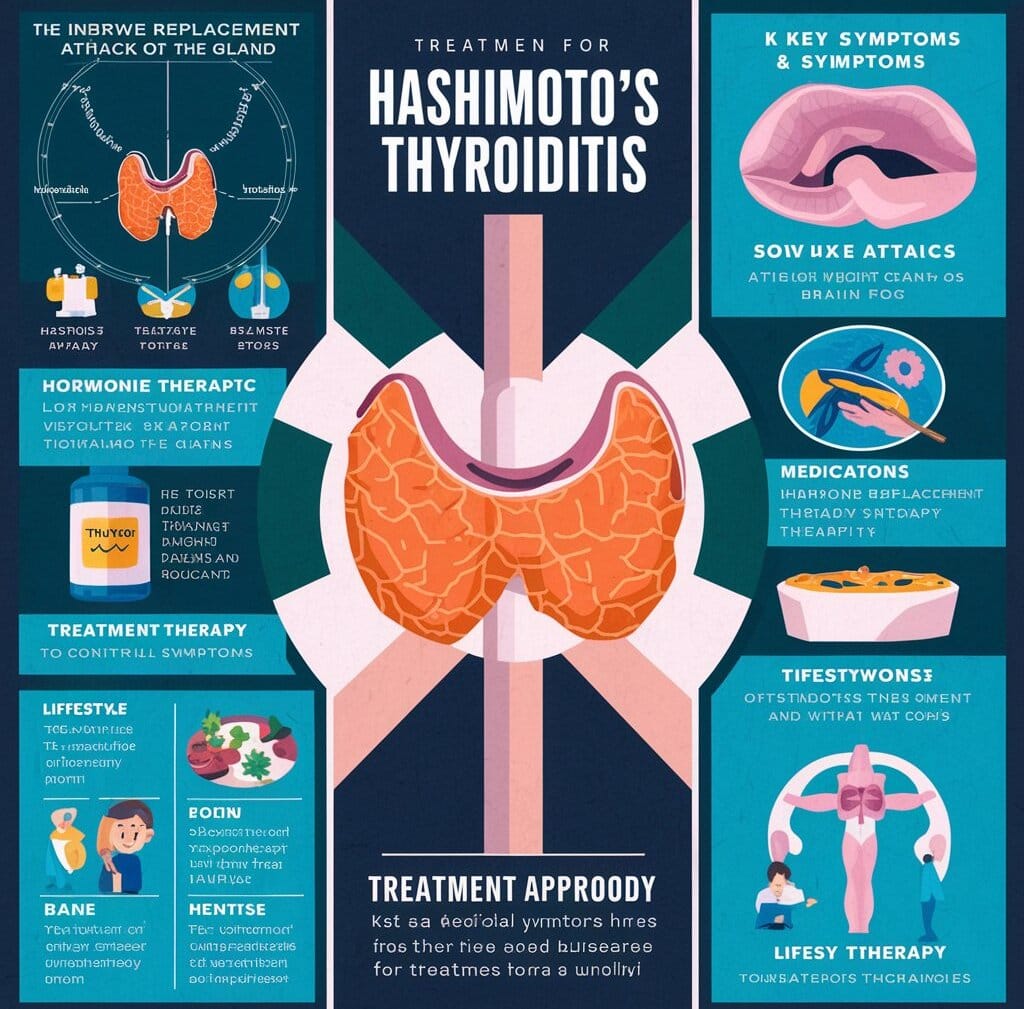
Hashimoto’s encephalopathy is a rare and poorly understood autoimmune disorder that affects the CNS, leading to a range of neurological symptoms. It is characterized by the presence of antithyroid antibodies, particularly antithyroid peroxidase (TPO) and antithyroglobulin (TG) antibodies, which are typically associated with Hashimoto’s thyroiditis, an autoimmune thyroid disease.
HE is a distinct entity from Hashimoto’s thyroiditis, although some patients may develop both conditions simultaneously. The symptoms of HE are diverse and can include cognitive impairment, seizures, stroke-like episodes, and neuropsychiatric problems. The pathophysiology of HE is not fully understood, but it is believed to involve the production of autoantibodies that target CNS components, leading to inflammation and damage.
The Connection Between MS and HE
There is, however, a surprising new connection between MS and HE. Recent studies have demonstrated the presence of a significant prevalence of antithyroid antibodies, especially TPO and TG antibodies, which are typical of HE in patients with MS. On the other hand, some patients with HE have also been described to demonstrating demyelinating lesions and other features that may reflect MS.
Several studies have demonstrated the coexistence of MS and HE:
- A 2018 study published in the journal Multiple Sclerosis and Related Disorders found that 24% of patients with MS had antithyroid antibodies, compared to 5% of healthy controls.
- A 2020 study published in the Journal of Neuroimmunology reported that 40% of patients with HE had demyelinating lesions consistent with MS.
- A 2019 review published in the Journal of Clinical Neuroscience noted that the coexistence of MS and HE is not uncommon, with some patients experiencing a simultaneous diagnosis of both conditions.
The exact mechanisms underlying the connection between MS and HE are unclear, but several theories have been proposed:
- Shared autoimmune mechanisms: Both MS and HE are characterized by an abnormal immune response, which may lead to the production of autoantibodies that target both the CNS and the thyroid gland.
- Common genetic susceptibility: Genetic factors may contribute to the development of both MS and HE, increasing the likelihood of co-occurrence.
- Environmental triggers: Exposure to environmental toxins, infections, or other triggers may contribute to the development of both conditions.
Implications and Future Directions
The connection between MS and HE has significant implications for diagnosis, treatment, and management. Healthcare providers should be aware of the potential for co-occurrence and consider screening for antithyroid antibodies in patients with MS, particularly those with atypical or treatment-resistant symptoms.
Further research is needed to fully understand the relationship between MS and HE, including the underlying mechanisms, epidemiology, and clinical features. The development of new diagnostic biomarkers and therapeutic strategies may also be necessary to address the complex needs of patients with both conditions.
Hashimoto’s Encephalopathy:
Hashimoto’s encephalopathy, also termed steroid-responsive encephalopathy associated with autoimmune thyroiditis, is a rare autoimmune disorder affecting the brain. It is defined as inflammation of the brain, usually associated with a background of Hashimoto’s thyroiditis.
The pathophysiology of Hashimoto’s encephalopathy remains unclear, but it is presumed to represent an autoimmune reaction against brain tissue in response to immune stimulation by thyroid antibodies. Symptoms of Hashimoto’s encephalopathy may be very variable and include confusional states, seizures, memory loss, hallucinations, and psychiatric disturbances.
The Connection:
While MS and Hashimoto’s encephalopathy are distinct conditions, there have been reported cases of individuals presenting symptoms of both simultaneously. The relationship between these two conditions is not yet fully understood, and research is ongoing to unravel the underlying mechanisms.
It is hypothesized that the autoimmune response in Hashimoto’s encephalopathy may contribute to the development or exacerbation of MS symptoms in individuals who already have MS. However, further studies are needed to establish a definitive link between the two.
Diagnosis and Treatment:
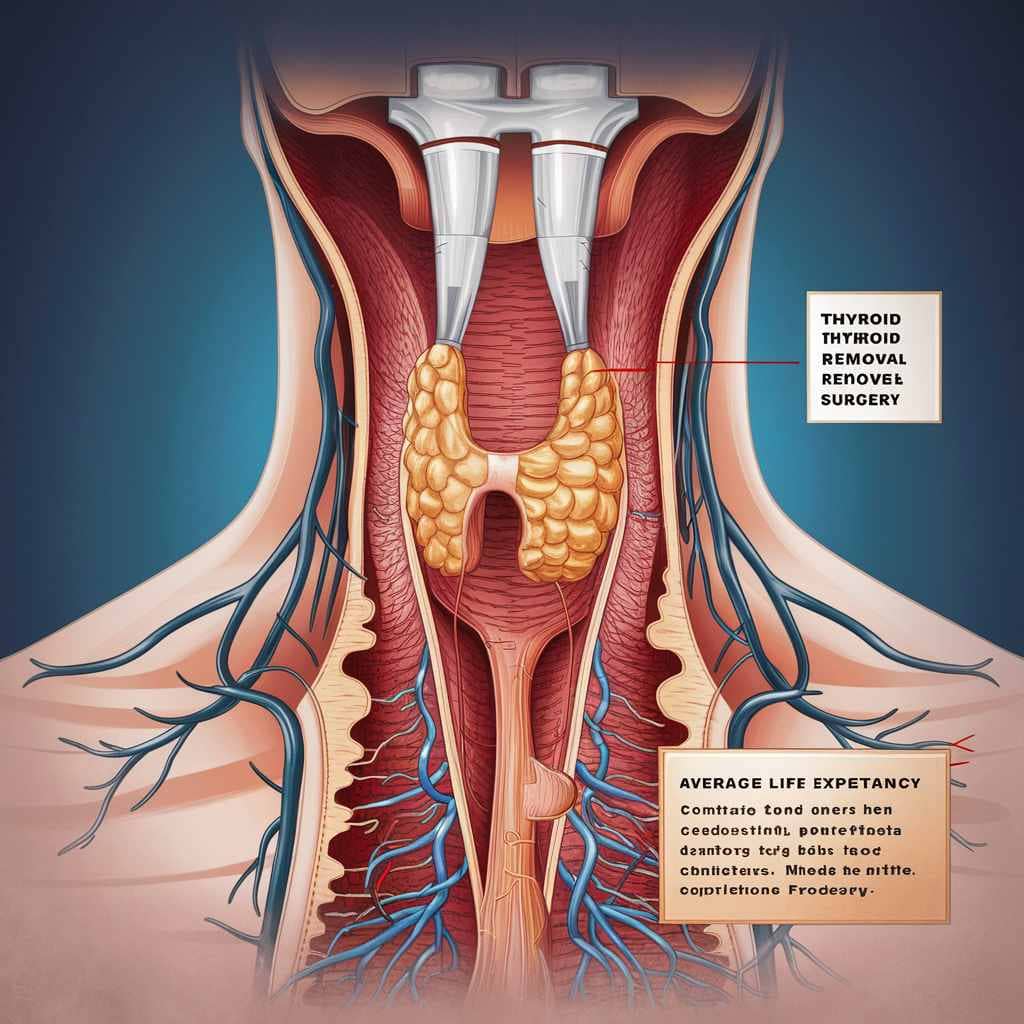
Diagnosing MS and Hashimoto’s encephalopathy requires a comprehensive evaluation of symptoms, a medical history, a physical examination, and various diagnostic tests. These may include MRI scans, blood tests, thyroid function tests, and cerebrospinal fluid analyses.
Treatment approaches for MS typically involve disease-modifying medications, symptom management, physical therapy, and lifestyle modifications. Hashimoto’s encephalopathy is often treated with high-dose corticosteroids to reduce brain inflammation and suppress the autoimmune response. In some cases, immunosuppressive medications may also be prescribed.
Conclusion
Multiple sclerosis and Hashimoto’s encephalopathy are two separate autoimmune conditions that affect the CNS in different ways. Though they have distinct pathophysiological mechanisms and clinical presentations, recent research shows an exciting connection between the two. The coexistence of MS and HE is not uncommon, and healthcare providers should be aware of the potential for co-occurrence. Further research is needed to understand the full relationship between MS and HE and to improve diagnosis, treatment, and management for patients suffering from these complex conditions.