Table of Contents
ToggleA Ray of Hope: Inspiring Graves’ Disease Remission Stories to Empower and Encourage
Graves’ disease is a disease resulting from an autoimmune response that leads to hyperactivity of the thyroid gland. Graves is the surname of Dr. Robert James Graves, who, belonging to an English background, presented the disease for the first time in 1835. This is a disease wherein the body is engulfed by the antibodies that fuel the thyroid gland to produce many of its hormones above normal. This way, a person may become confused and develop such common symptoms as a rapid pulse, tremors, rapid weight loss, and worry.
These first-hand accounts provide valuable insights and hope for others navigating similar health challenges.
-
Jamal Londry-Jackson
Jamal’s story is that of a survivor who is also a fighter. He survived and came out of the horrific experiences as an even more determined person. A growth in the neck gland right in 2015 was what he called “the option because of the active lifestyle.” Subsequently, during the hard workouts while playing football, he felt a visible lump, and to his surprise, his energy levels were lower.
He went to see the doctor, who was a thyroid specialist, who prescribed medication and advised him to see an endocrinologist. Finally, the endocrinologist administered drugs that held the gland growth; however, he missed that next visit. The regularity with which a patient took the medication might be the primary reason for his bad state of health. Taylor went through a second operation to have his thyroid gland removed in 2016, which he had done. His triumph signified someone who is resilient in the field as well as the place.
2. Christina Aragon
Five years down the line, Christina shares her musings after the diagnosis of Graves’ disease. She had symptoms that she combatted and remission that she achieved. What was appalling to Christina in the beginning was the lack of information. With her determination, she had to find ways to reverse the immunity. Her story was one of hope for others who were in the same state. She says, “It is possible to fight Graves’ disease if one learns the mechanism of this autoimmune disease and takes control.”
3. Ochie and Nikki
Graves’ disease would have kept them in the hospital, except they both beat the odds and miraculously entered remission. Ochie, almost conforming to remission, and Nikki, who have been symptom-free for a year, explain that a personalized protocol could result in the improvement of the condition. A regulatory expert with personalized attention and a proactive approach can be the key to the better prevention, detection, treatment, and management of chronic diseases.
Their interviews provide valuable insights for others on a similar path.
- Gemma’s Journey: Gemma’s story revolves around her struggle to get her thyroid levels under control before opting for surgery. Her perseverance and commitment to understanding her condition best exemplify the challenges Graves’ disease patients face. Her openness brought more awareness to people about thyroid disease and the effects that have a profound impact on individuals’ lives.
These stories sum up the bravery, determination, and strength of Graves’ disease sufferers. It shows that even though each of the stories is singular, they still point to the hope and motivation of those who have gone through this fight toward remission.
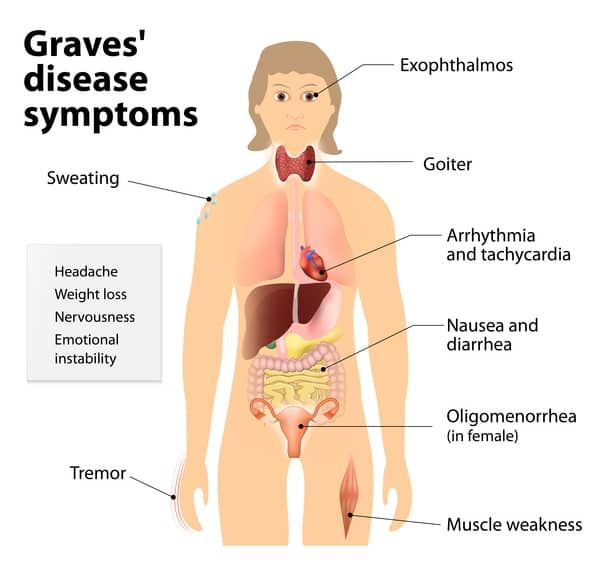
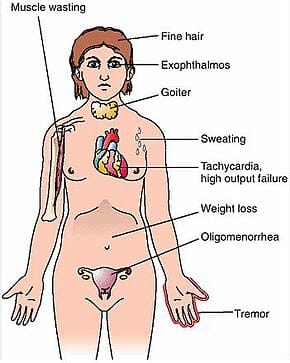
- Hyperthyroidism: Graves’ disease leads to excessive production of thyroid hormones. Common symptoms include:
- Weight loss: Despite a normal or increased appetite, individuals may lose weight.
- Increased heart rate (tachycardia): The heart beats faster than usual.
- Heat intolerance: sensitivity to warm temperatures.
- Tremors: fine trembling of the hands.
- Anxiety and restlessness: emotional changes due to elevated thyroid hormones.
- Fatigue: paradoxically, despite increased energy expenditure.
- Insomnia: difficulty falling asleep or staying asleep.
- Increased sweating: profuse sweating even in cool conditions.
- Enlarged Thyroid (Goiter): Graves’ disease often causes the thyroid gland to enlarge, leading to a visible swelling in the neck.
- Eye Changes (Graves’ Ophthalmopathy or Thyroid Eye Disease):
- Bulging eyes (exophthalmos): The eyes protrude forward due to inflammation of the eye muscles and tissues.
- Redness and irritation: Eyes may become red, dry, and painful.
- Double vision: due to pressure on the optic nerve.
- Swelling and puffiness around the eyes.
- Skin Changes:
- Pretibial myxedema: rarely, thickening and reddening of the skin on the shins.
- Acropachy: swelling and clubbing of the fingers and toes.
- Thyroid Storm (Rare): A life-threatening complication characterized by severe hyperthyroidism, high fever, rapid heart rate, and altered mental status.
- Other Symptoms:
- Menstrual irregularities: changes in menstrual cycles.
- Muscle weakness, especially in the upper arms and thighs.
- Brittle hair and nails are due to increased metabolic activity.
How is it diagnosed and treated?
- Diagnosis:
- Physical Examination: Your doctor will conduct a thorough physical exam, checking for signs and symptoms specific to Graves’ disease.
- Medical and Family History: Discussing your medical history and any family history of thyroid disorders helps in understanding the context.
- Blood Tests:
- Thyroid-Stimulating Hormone (TSH): Blood tests measure TSH levels. With Graves’ disease, TSH is usually low due to excessive thyroid hormone production.
- Free Thyroxine (T4) and Triiodothyronine (T3): Elevated levels of these hormones confirm hyperthyroidism.
- Thyroid Antibodies (TPO and TSI): The presence of these antibodies signifies an autoimmune process.
- Radioactive Iodine Uptake (RAIU): This test measures iodine uptake to assess thyroid function. Graves’ disease usually involves increased uptake.
- Thyroid Ultrasound: To evaluate thyroid size and detect nodules.
- Eye Examination: Especially if Graves’ ophthalmopathy (thyroid eye disease) is suspected.
- Treatment Options:
- Antithyroid Drugs:
- Methimazole (Tapazole) or Propylthiouracil (PTU): These drugs reduce thyroid hormone production. They are commonly used for symptom control and to prepare for other treatments.
- Radioiodine Therapy (I-131):
- Most Common Treatment in the United States: Radioactive iodine is swallowed, and it selectively destroys thyroid tissue. It leads to hypothyroidism, which can be managed with thyroid hormone replacement.
- Thyroidectomy (Surgery):
- Removal of the Thyroid Gland: Recommended in some cases for large goiters, intolerance to antithyroid drugs, or in cases of pregnancy.
- Partial or total thyroidectomy: Surgeons remove part or all of the thyroid gland.
- Beta-blockers are used to manage symptoms like rapid heart rate, tremors, and anxiety.
- Supportive Measures:
- Eye Care: Artificial tears, sunglasses, and elevating the head during sleep help manage eye symptoms.
- Nutrition and Lifestyle: A balanced diet, stress management, and avoiding iodine-rich foods (e.g., seaweed) are essential.
- Antithyroid Drugs:
- Monitoring and Follow-Up:
- Regular check-ups are crucial to assess thyroid function, adjust medications, and address any complications.
- Remission: Achieving remission (normal thyroid function) is the goal. Some individuals may remain on lifelong thyroid hormone replacement.

Remission of Graves’ disease varies from one person to another, but it is possible if managed properly. Let’s see what decides remission:
- Spontaneous Remission:
- Some people recover spontaneously without any treatment, but this is rare.
- Factors such as age, overall health, and the severity of the disease play a role.
- Treatment-Induced Remission:
- Antithyroid Drugs: These drugs—like methimazole or propylthiouracil—bring remission by lowering the production of thyroid hormones.
- Radioiodine Therapy (I-131): The most common treatment in the United States. It selectively destroys thyroid tissue, leading to hypothyroidism (an underactive thyroid).
- Thyroidectomy (surgery): surgical removal of part or all of the thyroid gland. Often results in remission.
- Factors Influencing Remission:
- Early Diagnosis: Timely intervention improves the chances of remission.
- The severity of hyperthyroidism: Mild cases may respond better to treatment.
- Individual Variation: Each person’s immune response and disease progression differ.
- Compliance with Treatment: Adherence to medication and follow-up appointments is crucial.
- Eye Involvement: Graves’ ophthalmopathy (thyroid eye disease) may impact remission.
- Monitoring and Follow-Up:
- Regular check-ups assess thyroid function and adjust treatment.
- Goal: Achieving stable thyroid function within the normal range.
- Long-Term Outlook:
- Some individuals achieve permanent remission, while others may experience relapses.
- Lifelong monitoring is essential, even after remission.
Conclusion
Graves disease usually presents a hard moment, but many patients experience remission with proper treatment. There is a possibility of describing different occurrences. However, Remission’s stories can be an example of hope and inspiration for someone making the same journey now. Higher care that is customized still has to be prescribed by a doctor for personalized use and supervision.